TOOTH EXTRACTION
The dentist who is going to extract a tooth must receive a full medical and dental history so that he can discover possible contraindications or, in general, all the factors that could possibly cause problems to the procedure or during the recovery time.
Special attention is required in cases of patients that receive anticoagulant therapy, where there must be a collaboration with the cardiologist regarding a possible temporary interruption of the therapy for some days before or even after the extraction, but principally in cases of patients that take bisphosphonates (drugs that intervene in bone regeneration and regard patients with severe osteopenia and patients with prostate/breast cancer), principally intravenously, where there must also be a collaboration with the treating physician regarding when an extraction can be performed, which depends on the dosage and the time period that the patient receives bisphosphonates.
When must an extraction take place?
In general, when a tooth is destroyed by dental caries, the dentist will try to restore it with a filling, or a root canal treatment and a crown, but there are cases where the tooth has sustained great damage and has very high mobility due to periodontal destruction and thus it cannot be cured. In this case, the only solution is the extraction of the tooth. Many times it is considered that a tooth should be extracted although the relevant conditions are not satisfied. It is recommended to visit a specialist dentist - endodontist so that there can be a proper evaluation. Root canal treatment-resection has now a very high rate of success, up to 99%, and thus even the most difficult teeth are saved.
Other reasons that can lead to the extraction of a tooth are the following:
- Deciduous teeth that are late falling out and prevent the eruption of permanent teeth.
- Patients undergoing orthodontic treatment who need to have some teeth extracted so that there is adequate space in order to arrange the rest of the teeth properly.
- Semi-impacted or impacted third molars need to be extracted when their eruption orientation is not favorable, when they have been affected by dental caries as they cannot always be easily accessed with the toothbrush and when the gums that surround them are swollen and hurt due to pericoronitis.
How is the extraction performed?
There are two types of extraction:
- The simple extraction, that regards teeth that have erupted in the mouth and which any dentist can perform. First the dentist uses an elevator (lever), a special instrument that loosens the connection of the tooth with the periodontal tissues and then uses the forceps, that is the instrument with which the tooth is finally extracted. Finally a cleaning of the gap socket (alveolus) is performed, that is of the space that remains after the extraction of possible residues of infected and inflamed tissues.
- The surgical extraction, which regards impacted teeth that have not erupted in the mouth, or broken teeth or remaining roots of teeth that are located at the same level or lower than the gums. The dentist with the proper instruments makes an incision in the gum and, if it is required, may remove some of the bone that surrounds the tooth in order to loosen it, or he may even split the tooth in two or in three. Finally, the cleaning of the socket is performed along with the stitching of the area, usually with absorbable sutures.
All extractions are performed with local or nerve block anesthesia in case of extraction of a tooth of the lower jaw, and what you feel during the extraction is a slight pressure, but there is no pain at all, if an adequate level of anesthesia has been achieved.
Do I need to take antibiotics after the extraction?
This depends on the dentist and is decided by him/her, depending on the case. The most common cases where antibiotics are required is when there is a large cyst and an abscess in the tooth that will be extracted, when the extraction is resistive, when the immune system is weakened due to a general disease, when there is a cardiovascular disease, such as prolapse etc, and it is always decided in collaboration with the treating physician.
What must I be careful of after the extraction? - instructions
In general, how you will feel after the extraction depends on the initial state of the tooth that has been extracted (for example, if there was a large abscess, etc), as well as if the extraction was resistive and lasted long.
You must always consider that the extraction of a tooth is a surgery and thus a mild discomfort after the operation is expected. In order to minimize this discomfort we always administer a painkiller-anti-inflammatory drug, while after the extraction the patient must systematically take painkillers for 2-3 days, and immediately after the surgery an ice pack is placed externally for 10 minutes so that the chances that an extraoral edema (swelling) occurs are minimized.
Furthermore, after the extraction, it is recommended to the patient to avoid smoking and performing any sucking motion (for example, sucking through a straw, spitting, etc) because the clot that begins to form immediately after the completion of the extraction will be dissolved and a mild bleeding will occur, which is quite undesirable at this phase. It is also good that the consumption of very hot beverages is avoided after the extraction and that cold and soft food is consumed on the day of the extraction. The patient can resume his eating habits on the very next day. Regarding oral hygiene, the patient shall begin to brush the extraction point on the fourth day after the extraction, while he can wash his/her mouth with a mouthwash that contains the antimicrobial agent chlorhexidine after the second day.
Finally, a re-examination of the patient must be performed a week after the extraction, so that the dentist can verify the normal healing of the area and remove the remaining sutures.
Which are the complications after the extraction?
One of the complications is the so-called dry socket, at a percentage of 5-10% of the cases, and mostly in rear teeth of the lower jaw. It can occur 2-3 days after the tooth extraction, is quite painful, is accompanied by oral malodor and it occurs when the socket, that is the location of the tooth in the jaw before extraction, gets infected and does not heal because of the lack of formation of a clot. The clot is the mass of coagulated blood and is formed at the spot (socket) where the extraction was performed and in this way the human body begins to restore the wound that has been made by the extraction. Therefore, the absence of this clot means that the wound is not closed and that the bone in which the roots of the tooth lied remains exposed to the environment of the mouth and gets infected. The causes to which this is due are mainly: smoking immediately after the extraction, bad oral hygiene, sucking of the wound, the lack of vitamins C and D. Its treatment includes medication consisting of painkillers-anti-inflammatory drugs and daily rinsing of the wound by the dentist with a special preparation that contains the soothing agent eugenol; with this treatment the improvement is spectacular from the first day.
In any case and in order to avoid extractions, it is good that the patient takes care of his own oral hygiene and that he is examined every 6 months by his/her dentist, so that all his teeth can remain in his mouth, as the desired outcome is that we all have a healthy functional mouth and a beautiful smile.
Constantinos Laghios, Dental Surgeon - Endodontist, M.S. - Christina Kotsiopoulou, Dental Surgeon.
Tooth with huge lesion: Extraction, placement of bone graft and subsequently implant had been advised by a specialist

Root canal treatment with incision of the abscess was done. Eleven months recall shows complete bone healing

1.A decayed tooth with a doubtful , problematic root canal treatment
2.Initial x-ray with an incorrect, unfinished root canal treatment, in a patient currently facing serious pain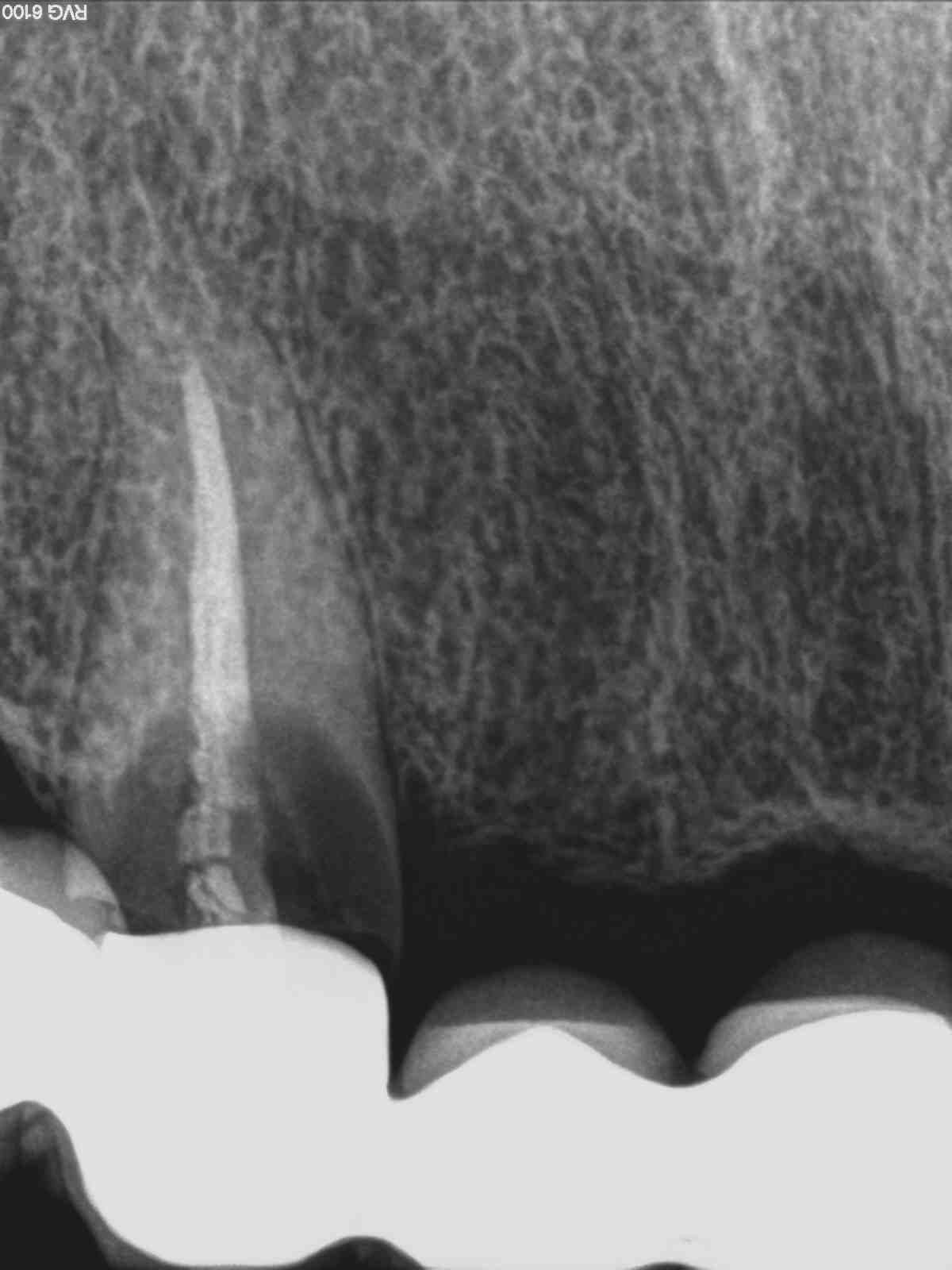
3.Α correct root canal treatment processed through a high-tech “Carl Zeiss” dental microscope
4.A successful root canal retreatment, reaching the very last millimeter of the apex
5.Flap
6.Placement-adhesion of a post
7.Placement of resin composite
8.1-week recall: we can notice that the successfully endodontically treated tooth remains as an abutment in the existent bridge without being
necessary to replace the old bridge with a new one so the patient avoided any possible discomfort and financial burden as well